Local Anesthetic Systemic Toxicity (LAST)
While the effects of LAST have been recognized since the late 1880's, it wasn't until George A. Albright, M.D. published a seminal editorial that what was perhaps once whispered about among colleagues, was now brought out into the light.
Classic description of LAST found in most textbooks:
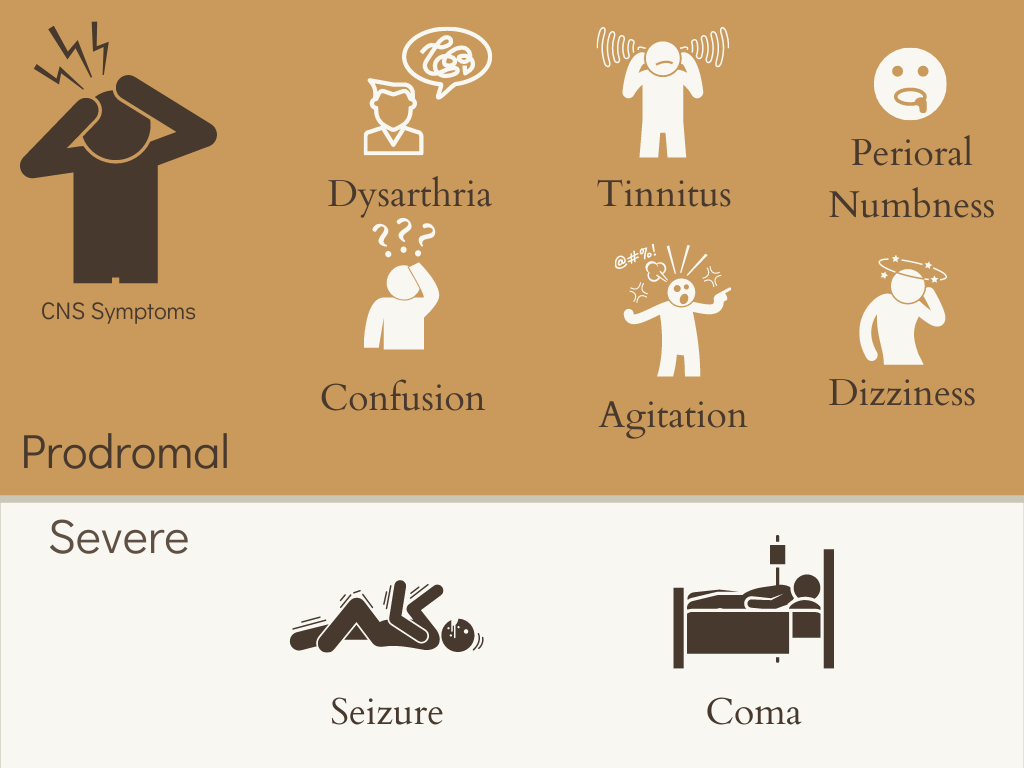
1. An initial prodromal phase with progressively worsening neurologic signs including dysarthria, perioral numbness, confusion, dizziness, ultimately culminating in seizures and coma.
2. Onset of symptoms is classically immediately after injection of LA.
3. In extreme cases of systemic toxicity, signs of hemodynamic instability follow and can lead to cardiovascular collapse and death.
A variety of factors influence the likelihood and severity of LAST, including individual patient risk factors, block location and technique, specific local anesthetic, total dose, timely recognition, and the effectiveness of interventional treatment. The incidence of LAST is roughly around 0.03% per block performed, with over 1/5th of cases occurring outside of the traditional hospital setting, and 50% occurring in the hands of non-anesthesiology specialists.
Pathophysiology in LAST
Local anesthetic agents work by attaching to the intracellular domain of the Na+ channel, thereby inhibiting neuronal ion transfer and depolarization, and preventing neuronal transmission. This works great if you are selectively targeting sensory nerves, but larger doses will be redistributed systemically, affecting unintended target locations.
In the central nervous system, local anesthetics initially impair inhibitory pathways, leading to unopposed excitatory effects experienced as sensory/visual changes, muscular activation, and seizure activity. As the concentration of local anesthetic rises, the excitatory pathways are also subsequently impaired, eventually leading to loss of consciousness, coma, and respiratory arrest.
Local anesthetics effects on the cardiovascular system are primarily by direct Na+ channel blockade, which results in rhythm disturbances. Secondary effects of LA toxicity may include myocardial dysfunction, such as decreased contractility, as well as labile vascular tone.
Signs and Symptoms
Di Gregorio et al reviewed the published reports of LAST spanning over 30 years. They identified 93 cases associated with regional anesthesia. Neurologic signs or symptoms were present in almost 90% of cases. Seizure, agitation, and loss of consciousness were the most frequent signs of CNS toxicity, while prodromal symptoms were far less common, occurring in only about 15% of reported cases. Cardiovascular symptoms occurred in about 55% of patients, with bradycardia and hypotension typically presenting as the initial sign. While neurologic symptoms occurred in the vast majority of cases, a small percentage of patients presented solely with cardiovascular symptoms.
The majority of cases occurred after single injections, with 55% related to bupivicaine.
While the onset of signs occurred in less than 1 min in the majority of cases, in about 25% it took between 1- 5 minutes, and in over 10% of cases it took more than 10 minutes for symptoms to appear.
Surprisingly, the greatest time interval for onset of symptoms was 60 minutes!
While the classic description of LAST begins with prodromal CNS symptoms and rapidly progresses to also include CV symptoms, over 40% of published case reports were atypical, with either a delayed presentation or devoid of CNS symptoms entirely. The findings of DiGregorio et al challenge the classic presentation and argue for increased vigilance. Their findings are especially prescient, as the vast majority of our blocks are routinely performed under deep sedation or general anesthesia in children, which may mask CNS symptoms, especially if paralytics are used.
Prevention of LAST
There is no single measure that can prevent LAST in clinical practice. Having said that, there are some things that one can do that may reduce the likelihood of progressing to toxic levels:
Ultrasound guidance may reduce the incidence, as one can more precisely target (and avoid vasculature)
Use the lowest effective dose of local anesthetic (dose = volume x concentration)
Incremental injection of local anesthetics, pausing between each injection (one circulation time)
Aspirate before each injection (bear in mind there is a 2% false-negative rate for this diagnostic intervention)
When injecting potentially toxic doses of local anesthetic, one can use of an intravascular marker. In the largest study to date, PRAN prospectively evaluated almost 100,000 blocks, the majority under GA (93.7%). In a little over 8 years, they had 7 cases of LAST. The use of an intravascular marker did not reduce the risk of LAST, as epinephrine has been shown to have a limited (-) predictive value. Having said that, although epinephrine is an imperfect maker, its benefits likely outweigh its risks in the majority of patients. It was noted that there were 80 reported positive test doses, and given the high positive predictive value of the test dose, it is possible that many cases of LAST were avoided.
Treatment Recommendations
For many years, the mainstay of treatment for LAST was supportive. Airway management, seizure control, ACLS, and even cardiopulmonary bypass have all been used to treat suspected toxic doses of local anesthetics. Through the pioneering work of Guy Weinberg and collaborators, a therapeutic breakthrough for local anesthetic-induced cardiac arrest was discovered: lipid emulsion therapy, or intralipid. In their work, Weinberg et al successfully used intralipid to resuscitate both rats and dogs exposed to toxic doses of bupivicaine. The exact mechanism of how this occurs remains unclear.
In a striking moment of recollection, presence of mind, and a flash of insight—a coup d'oeil if you will— Rosenblatt et al successfully used Intralipid 20% to resuscitate a patient from a prolonged cardiac arrest that immediately followed the placement of an interscalene block. Prior to this, intralipid had never been used in humans as a resuscitative therapy in suspected cases of local anesthetic overdose. This clinical leap revolutionized the treatment of LAST and ushered in a new era of precaution. Much like dantrolene for malignant hypothermia, intralipid is now considered a “crucial antidote” and is routinely kept in areas where local anesthetics are used.
To date, there are no published recommendations regarding lipid emulsion dosage in children, though intralipid has been successfully used in children of all ages, including neonates. Protocols have been adapted using adults as a reference.
Butterworth, J.F., 2010. Models and mechanisms of local anesthetic cardiac toxicity: a review. Regional anesthesia and pain medicine, 35(2), pp.167-176.
Mulroy, M.F. and Hejtmanek, M.R., 2010. Prevention of local anesthetic systemic toxicity. Regional anesthesia and pain medicine, 35(2), pp.177-180.
Di Gregorio, G., Neal, J.M., Rosenquist, R.W. and Weinberg, G.L., 2010. Clinical presentation of local anesthetic systemic toxicity: a review of published cases, 1979 to 2009. Regional anesthesia and pain medicine, 35(2), pp.181-187.
Chazalon, P., Tourtier, J.P., Villevielle, T., Giraud, D., Saïssy, J.M., Mion, G. and Benhamou, D., 2003. Ropivacaine-induced cardiac arrest after peripheral nerve block: successful resuscitation. The Journal of the American Society of Anesthesiologists, 99(6), pp.1449-1451.
Walker, B.J., Long, J.B., Sathyamoorthy, M., Birstler, J., Wolf, C., Bosenberg, A.T., Flack, S.H., Krane, E.J., Sethna, N.F., Suresh, S. and Taenzer, A.H., 2018. Complications in pediatric regional anesthesia: an analysis of more than 100,000 blocks from the pediatric regional anesthesia network. Anesthesiology, 129(4), pp.721-732.
Weinberg, G.L., 2010. Treatment of local anesthetic systemic toxicity (LAST). Regional anesthesia and pain medicine, 35(2), pp.188-193.
Rosenblatt, M.A., Abel, M., Fischer, G.W., Itzkovich, C.J. and Eisenkraft, J.B., 2006. Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest. Anesthesiology: The Journal of the American Society of Anesthesiologists, 105(1), pp.217-218.
Lönnqvist, P.A., 2012. Toxicity of local anesthetic drugs: a pediatric perspective. Pediatric Anesthesia, 22(1), pp.39-43.
Shah, S., Gopalakrishnan, S., Apuya, J., Shah, S. and Martin, T., 2009. Use of Intralipid in an infant with impending cardiovascular collapse due to local anesthetic toxicity. Journal of anesthesia, 23(3), pp.439-441.
Presley, J.D. and Chyka, P.A., 2013. Intravenous lipid emulsion to reverse acute drug toxicity in pediatric patients. Annals of Pharmacotherapy, 47(5), pp.735-743.
Neal, J.M., Bernards, C.M., Butterworth IV, J.F., Di Gregorio, G., Drasner, K., Hejtmanek, M.R., Mulroy, M.F., Rosenquist, R.W. and Weinberg, G.L., 2010. ASRA practice advisory on local anesthetic systemic toxicity. Regional anesthesia and pain medicine, 35(2), pp.152-161
El-Boghdadly, K., Pawa, A. and Chin, K.J., 2018. Local anesthetic systemic toxicity: current perspectives. Local and regional anesthesia, 11, p.35.
Bosenberg, A., 2019. ESRA19-0693 Paediatric regional anaesthesia and last.
Bacon, B., Silverton, N., Katz, M., Heath, E., Bull, D.A., Harig, J. and Tonna, J.E., 2019. Local anesthetic systemic toxicity induced cardiac arrest after topicalization for transesophageal echocardiography and subsequent treatment with extracorporeal cardiopulmonary resuscitation. Journal of cardiothoracic and vascular anesthesia, 33(1), pp.162-165.